January 21, 2025
4 minimum read
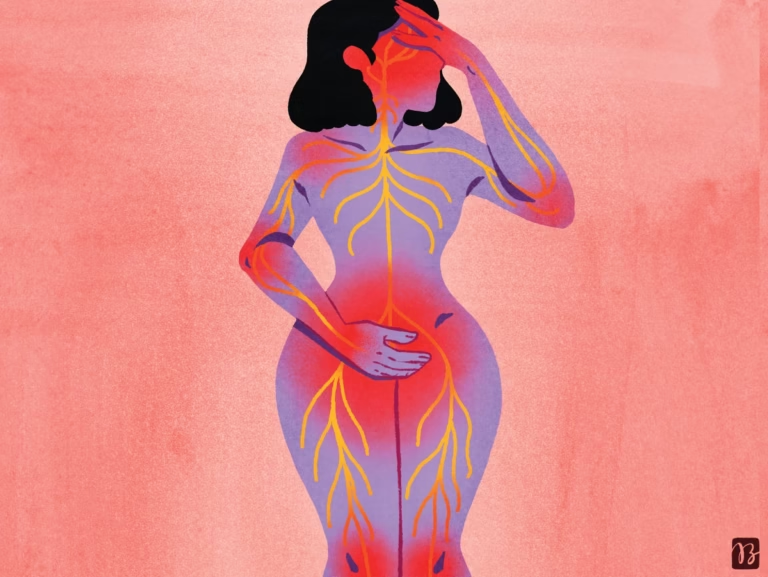
Painful endometriosis can affect the whole body, not just the pelvis
The disease is now thought to be genetically linked to widespread inflammation, asthma, and migraine headaches.

The pain of endometriosis, which affects an estimated 1 in 10 Americans born female, can be severe. Some people are unable to work or attend school. However, many doctors do not recognize the symptoms. On average, it takes 7 to 9 years for patients to receive a diagnosis.
This alarming statistic, along with the general lack of knowledge about endometriosis, is a powerful example of the gap in knowledge about women’s and men’s health. There is limited funding and research into what causes endometriosis and who is most at risk. This situation is finally starting to change, in part because the understanding of endometriosis is changing. It is not a purely gynecological disease. “In the last three to five years, this disease has been completely reframed as a systemic neuroinflammatory disease,” said Philippa Saunders, a reproductive biologist at the University of Edinburgh. “It wasn’t just a little tissue stuck in the wrong place. My whole body reacted.”
Endometriosis, which involves tissue in the uterus, begins in a process known as retrograde menstruation, when menstrual blood flows backwards up the fallopian tubes and into the pelvis. Blood contains fragments of the endometrial tissue that lines the inside of the uterus. In some cases, this tissue, rather than being cleared by the immune system, attaches to the ovaries or pelvic lining and then grows to create its own blood supply. This lesion can cause infertility as well as debilitating pain. “We’re not talking about a little bit of pain here,” Sanders says. “(People) can’t function.” And unlike menstrual pain that occurs during menstruation, endometriosis pain can come back at any time.
About supporting science journalism
If you enjoyed this article, please consider supporting our award-winning journalism. Currently subscribing. By subscribing, you help ensure future generations of influential stories about the discoveries and ideas that shape the world today.
The medical profession’s habit of limiting health issues to narrow silos (traditionally, only gynecologists saw patients with endometriosis) is not helping. “We fragment human health into disciplines and systems, but[these systems]are much more interconnected than we expected,” said Stacey Mismer, a reproductive biologist at Michigan State University. I realized that we are connected.” She points out that endometriosis causes symptoms and consequences that affect many other parts of the body.
For example, adolescents and young women with endometriosis are five times more likely to be diagnosed with irritable bowel syndrome than women without endometriosis. Although cardiovascular events are rare in all women under 60, women with endometriosis have a relative risk of hypertension, stroke, angina or heart attack of 20%, depending on the study and condition. ~80% increase. Patients have twice the risk of rheumatoid arthritis, and patients with endometriosis have a higher prevalence of asthma, lupus, and osteoarthritis. These people are more likely to suffer from multiple medical conditions such as migraines, lower back pain, and fibromyalgia, a chronic pain condition.
Scientists still cannot say for sure why these symptoms often occur together. “We think one of the important pathways is chronic inflammation,” Mismer says. For example, affected people may have an inflammatory response to certain triggers common to several diseases.
Researchers know that about half of the risk of endometriosis is due to genetic factors. Early research has identified common high-risk genes for the condition, namely; BRCA Breast Cancer Genes – Recent large-scale studies suggest genome-wide genetic variations. 2023 Survey natural genetics A study of about 60,000 people with endometriosis and more than 700,000 people without endometriosis found more than 40 locations in the genome that have changes associated with a higher risk of endometriosis. “This is a huge leap forward in our understanding,” says Krina Zondervan, a genetic epidemiologist at the University of Oxford.
In the same study, this leap allowed researchers to focus on the common biology of several diseases that often co-occur with endometriosis. For example, we have discovered links between endometriosis and the underlying genetics of other types of pain, such as migraines. These pain conditions trigger a biological process called central sensitization. This occurs when chronic pain changes the central nervous system’s response to painful stimuli. Many of the genes involved are related to pain perception and maintenance. They also found a link with inflammatory conditions such as asthma.
What may help with diagnosis and treatment is the recent recognition that endometriosis is not a single disease. This is a condition that has three subtypes. Ovarian endometriosis, which affects the ovaries, is most commonly inherited. Deep endometriosis invades deep into the pelvis and forms very hard nodules. In peritoneal or superficial endometriosis, small lesions are more diffusely scattered along the pelvic lining. As with breast cancer, subtypes are likely to have different risk factors.
Until recently, the only way to diagnose endometriosis was through laparoscopic surgery. However, less invasive methods are now being used. For example, ultrasound imaging can detect ovarian endometriosis, and MRI scans can reveal deep lesions. Unfortunately, imaging tests have not yet performed well for the most common type of peritoneal endometriosis. Patients also need to be referred for such imaging tests, which are not available to all due to misdiagnosis and inequity in access to care.
Treatment is to surgically remove the lesion, which is effective for some but not all patients. Identifying accompanying symptoms can determine who can’t be helped. People who suffer from pain that extends beyond the pelvis may not benefit from surgery. “There’s nothing to cut,” Mismer said. A clinical trial is underway in the UK to study outcomes with and without surgery.
Anyone who has been diagnosed with endometriosis or has worrisome symptoms should talk to their doctor as well as their gynecologist now. This is not a problem with one part of the body.
This is an opinion and analysis article and the views expressed by the author are not necessarily those of the author. scientific american.