August 16, 2024
4 Time required to read
One in four people who are unresponsive with brain injuries may be conscious
Research suggests that more people in a coma or similar state can hear what’s going on around them than we thought.
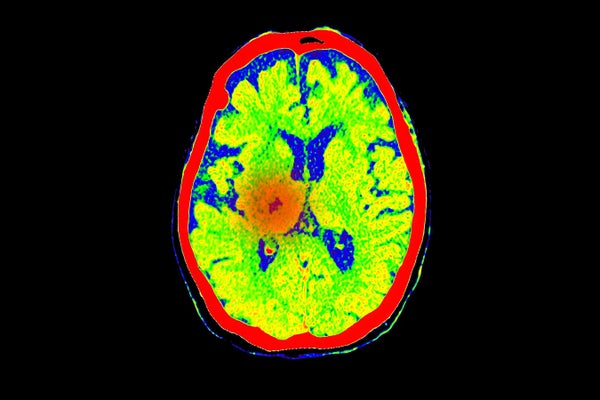
Brain scans show blood flow in the area where a stroke, a common cause of coma, has occurred.
Mr. Supachai praserdumrongchai/Getty Images
At least a quarter of people with severe brain injuries who are physically unable to respond to commands are actually conscious, according to the first international study of its kind.
These people, for example, were unable to give a thumbs up when prompted, yet repeatedly showed brain activity when asked to imagine themselves moving or exercising.
“This is one of the great breakthroughs in the field of coma and other disorders of consciousness,” said Daniel Kondziela, a neurologist at Rigsspitalet, Copenhagen University Teaching Hospital.
Supporting science journalism
If you enjoyed this article, please support our award-winning journalism. Subscribe. By purchasing a subscription, you help ensure a future of influential stories about the discoveries and ideas shaping the world today.
The results mean that many brain-injured patients who appear unresponsive may be able to hear what’s going on around them and even communicate using a brain-computer interface (BCI), says study leader Nicholas Schiff, a neurologist at Weill Cornell Medicine in New York City. A BCI is a device implanted in a person’s head that captures and decodes brain activity, translating it into commands that can, for example, move a computer cursor. “We should be allocating resources to finding these people and helping them,” Schiff says. The study was published August 14. New England Journal of Medicine.
The study involved 353 people who had suffered brain damage from events such as physical trauma, heart attack or stroke. Of these, 241 did not respond to any of a battery of standard bedside reaction tests, including the thumbs-up gesture, but the remaining 112 did.
Everyone in the study underwent one or both of two types of brain scans. The first was functional magnetic resonance imaging (fMRI), which indirectly measures mental activity by detecting blood oxygenation in the brain. The second was electroencephalography (EEG), which directly measures brainwave activity by placing a cap covered with electrodes on a person’s scalp. During each scan, subjects were instructed to imagine themselves playing tennis, opening and closing their hands. The instructions were repeated continuously for 15 to 30 seconds, then a pause, and then the exercise was repeated for six to eight sessions of instructions.
Of those who were physically unresponsive, about 25 percent showed brain activity throughout the EEG or fMRI scan. Being able to respond mentally but not physically is medically known as cognitive-motor dissociation. The 112 people the study classified as responsive did a little better on brain activity tests, but not by much; only 38 percent showed activity consistently. That’s probably because the tests are so demanding, Schiff says. “I’ve done this experiment where I went into an MRI, and it was hard,” he adds.
This isn’t the first study to show cognitive-motor dissociation in physically unresponsive people with brain injuries: A 2019 paper, for example, found the behavior was present in 15 percent of 104 people tested. But the latest study is larger and the first multicenter study of its kind. Tests were conducted at six medical centers in four countries: Belgium, France, the UK, and the US.
The 25% of non-responders who showed brain activity tended to be younger than non-responders, to have sustained injuries from physical trauma, and to have lived with their injuries longer than others. Conziera cautions that further exploration of these associations will require repeated assessments of individuals over weeks or months. “We know very little about the trajectory of consciousness recovery over time and across different brain injuries,” he says.
However, the study has some limitations, such as the number and set of tasks used by the medical centers during the EEG and fMRI scans not all being the same, and the number of electrodes used during the EEG sessions was not the same, which could skew the results.
But ultimately, Schiff says, the bar is so high to record brain activity that the study likely underestimates the percentage of people who are conscious but not physically responsive. Conziera agrees: He notes that rates of cognitive-motor dissociation were highest in people who were tested with both EEG and fMRI, and the overall rate could have been even higher if everyone in the study had used both methods.
But the types of tests used are logistically and computationally challenging, “which is why only a handful of centers around the world have the capacity to deploy these technologies,” Conziera says.
Schiff stresses the importance of being able to identify people who have suffered brain injuries and are conscious even when they appear unresponsive. “There will be someone who can help get them out of this,” he says, perhaps with a BCI or other therapy, or simply through continued medical care. Knowing that someone is conscious can change decisions that families and medical teams make about life support and treatment. “Any time you know someone is responsive, it changes things,” he says.
This article is reprinted with permission. First Edition August 14, 2024


2 Comments
Can you be more specific about the content of your article? After reading it, I still have some doubts. Hope you can help me.
Your article helped me a lot, is there any more related content? Thanks!